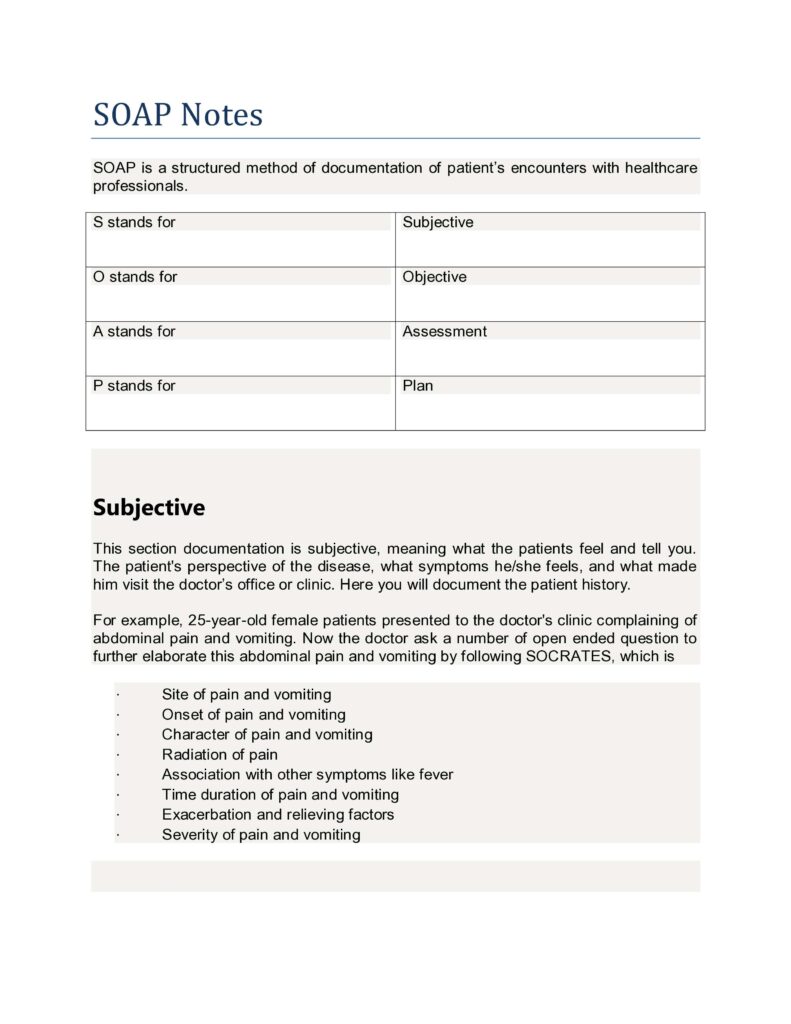
SOAP is an acronym for
- S for Subjective
- O for Objective
- A for assessment and
- P for plan.
This is a widely used formula for documenting patient encounters with the doctor.
This formula makes it easy to record the patient and doctor coverage in a step-wise manner.